 ‘Blurbs’ made a welcome return to Brasenose on Wednesday evening of 4th week. Named after publishers’ dust-jacket summaries of a book’s contents, the usual format consists of two short presentations by members of the Senior Common Room (SCR) and Graduate or Hulme Common Room (HCR). Always varied and never predictable, the inaugural Blurbs of Term was, however, an all-SCR affair devoted to Medicine. Professors Bleddyn Jones (Gray Laboratory, Cancer Research UK Oxford Centre) and Ted Wilson (for many years Head of the CERN Accelerator School and now Visiting Prof at Oxford Physics Department's John Adams Institute) gave complementary talks on Proton Beam Therapy.
‘Blurbs’ made a welcome return to Brasenose on Wednesday evening of 4th week. Named after publishers’ dust-jacket summaries of a book’s contents, the usual format consists of two short presentations by members of the Senior Common Room (SCR) and Graduate or Hulme Common Room (HCR). Always varied and never predictable, the inaugural Blurbs of Term was, however, an all-SCR affair devoted to Medicine. Professors Bleddyn Jones (Gray Laboratory, Cancer Research UK Oxford Centre) and Ted Wilson (for many years Head of the CERN Accelerator School and now Visiting Prof at Oxford Physics Department's John Adams Institute) gave complementary talks on Proton Beam Therapy.
During the summer vacation, the heart-rending story of Ashya King (a five-year-old child whose life is threatened by a brain tumour) made national headlines after his parents removed their son from hospital and travelled to first Spain and then Prague in search of a therapy described as ‘controversial’ in many media accounts. Professors Wilson and Jones explained the fundamentals lying behind radical cancer treatment to a mixed audience of graduates studying for taught and research masters in science, humanities, and social science subjects.
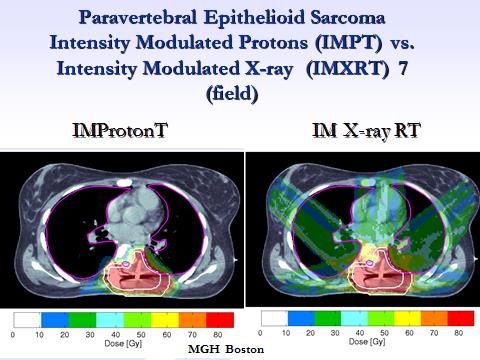
The technology underpinning CERN’s Large Hadron Collider at lower energy levels generates beams that are used in medical cyclotrons and synchrotrons. Radiations have different biological qualities, the energy deposition profile of X-rays differing greatly from that of protons. As velocity declines, the energy dissipated by protons rises sharply to reach what is known as a Bragg peak. Proton treatment, therefore, results in less damage to many normal tissues than X-ray ionising radiation provided that it is targeted accurately. Medics choosing between the two techniques face difficult trade-offs, particularly in cases where a cancer is located near to vulnerable body parts such as the spinal cord, the brain, or the eye. X-ray treatment results in greater collateral dose to non-affected areas, but misdirected proton beams carry the risk of causing, for example, later brain damage, paralysis, or blindness after treatment of some forms of brain tumours. Calibrating proton treatment is extremely challenging: even the act of breathing can result in a misdirected beam. Judging the relative biological effectiveness (RBE) of one type of ionised radiation relative to another is greatly complicated by limited experimental data of different types of animal and human tissue. There is at the present time international disagreement about the use of a constant RBE (as used in American practice) versus a variable RBE with dose, in different tissues and for different tumour types as favoured in Oxford.
Questions from the floor to the two speakers discussed the advantages and disadvantages of radical cancer therapy being subject to a light regulatory regime in comparison with pharmaceuticals. Tighter regulation would restrict treatment only to cases where tissue weighting factors are robust empirically, and would impose additional costs on industry or medical research funders such as charities. Yet while this would reduce the incidence of side effects, the gains must be offset against much slower development of techniques that offer significant benefits to patients. Professors Wilson and Jones hoped that the international collaborative research effort devoted to particle physics may soon be applied to medicine. 3-D humanoid phantom dosimetry, in which one of CERN’s synchrotrons will be used to investigate the properties of beams within synthetic human tissue types and for cell based experiments, promises to make proton beam therapy a safer and better option for children like Ashya with medulloblastoma.
